Minimally Invasive Medicine
Interventional Radiology (IR) is a selection of advanced techniques and medical procedures that use imaging equipment to treat various illnesses. Interventional radiologists are physicians who specialize in these minimally invasive, targeted treatments performed using imaging guidance. These physicians use their expertise in interpreting X-rays, ultrasound, magnetic resonance imaging (MRI), and computed tomography (CT) to diagnose and treat disease.
Advantages
Interventional Radiology techniques are an advance in medicine that often replace open surgical procedures and are typically much less invasive. They are generally easier for the patient because they involve no large incisions, less risk, less pain, and shorter recovery times.
At MIIGS, making patients better faster is our top priority.
- Most procedures can be performed on an outpatient basis or require only a short hospital stay.
- General anesthesia is usually not required.
- Risk, pain and recovery time are often significantly reduced.
- Procedures often replace surgery and are typically much less invasive.
Common Procedures
MIIGS’s board certified physicians perform a variety of interventional radiology-based procedures, treatments and pain management techniques. Choose a procedure in the list to the left for more information.
Overview
There are a variety of procedures that can be performed to help alleviate the symptoms of back pain. A few of these include Epidural Steroid Injections, Facet injections, and Nerve Root Blocks.
Epidural Steroid Injections
MIIGS doctors use fluoroscopy to help guide the needle into the epidural space, and the medicine is injected directly into the epidural space. Controlled studies have found that medication is misplaced in 13% to 34% of all epidural injections that are performed without fluoroscopy.
An epidural spinal injection (ESI) may be performed when one or more nerve roots are affected or if the pain is on both sides of the back or leg. With an ESI the steroid is injected directly into the epidural space. The epidural space is the area that surrounds the spinal cord and the nerves coming out of it. A small needle is guided into the epidural space under fluoroscopy guidance. This guidance greatly increases the success of the procedure over traditional non-imaging guided techniques. The injections are usually performed in sets of three, with each injection occurring one week apart.
Facet Joint Injections
The injection of local anesthetic and steroids into the facet joint is diagnostic and potentially therapeutic. Pain relief following a precise Intra-articular injection confirms the facet joint as a source f pain. The injection of steroids provides longer pain relief. Long-term relief (approximately 6 months) can be obtained in 50-70% of patients.
Nerve Root Injections
Nerve root blocks are useful to diagnose and treat back pain. Nerve root blocks can be used to anesthetize the desired nerve for diagnostic and therapeutic purposes. Once the symptomatic nerve root is known, targeted steroid injections are used in an attempt to produce long-term relief, primarily in patients with radiculopathy.
Multiple causes of radiculopathy have been discovered. It is usually the result of pressure on or inflammation around the nerve root. This causes pain within the nerve root, which is referred to along the course of the nerve (radiculopathy). Because steroids have an anti-inflammatory action, injections around the nerve root may reduce inflammation, thereby decreasing or eliminating the pain.
Overview
Needle biopsy is commonly used to identify the cause of a lump or mass or other abnormal conditions in the body.
During the procedure, the doctor inserts a small needle guided by X-rays, ultrasound, or a CT scan. The needle is guided into the abnormal area. A sample of tissue is removed and given to the pathologist for review. The needles used are typically very small and there is minimal to no pain associated with the biopsy.
Overview
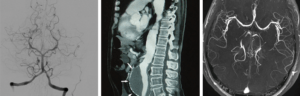
Angiography is a type of X-ray performed to image blood vessels in various parts of the body, including the legs, heart, brain and kidneys. This is performed in order to determine whether the vessels are diseased, narrowed, enlarged or blocked all together.
Angiography, CT Angiography, Ultrasound & MR Angiography
MIIGS doctors use a variety of less invasive methods, such as computed tomography (CT) angiography and magnetic resonance (MR) angiography. In addition, catheter angiography is also performed on patients who may undergo surgery, angioplasty, or stent placement. After passing a catheter through an artery leading to the body area of interest, contrast material is injected into the arteries in order to highlight the vessels when X-rays are taken. If an area of narrowing or blockage is seen this can be treated using minimally invasive technique such as angioplasty and/or stent placement.
Overview
An aortic aneurysm is a weak area in the aorta-the main blood vessel that carries blood from the heart to the rest of the body. As blood flows through the aorta, the weak area bulges like a balloon and can burst if the bulge gets too big. Once an aneurysm reaches 5 cm in diameter, it is usually considered necessary to treat the aneurysm in order to prevent rupture. Below 5 cm, the risk of aneurysm rupturing is lower than the risk of interventional surgery in patients with normal surgical risks. The goal of therapy for aneurysms is to prevent them from rupturing. Once an abdominal aortic aneurysm has ruptured, the chances of survival are low, with 80-90% of all ruptured aneurysms resulting in death. These deaths can be avoided if an aneurysm is detected and treated before it ruptures
Abdominal aortic aneurysms can now be repaired using minimally invasive techniques. This minimally invasive technique is performed by interventional radiologists using imaging to guide the catheter and graft inside the patient’s artery, rather than making a large incision. For the procedure, an incision is made in the skin at the groin through which the catheter is passed into the femoral artery and directed to the aortic aneurysm. Through the catheter, the physician passes a stent graft that is compressed into a small diameter within the catheter. The stent graft is advanced to the aneurysm and then opened, creating new walls in the blood vessel through which blood flows.
This is a less invasive method of placing a graft within the aneurysm to redirect blood flow and stop direct pressure from being exerted on the weak aortic wall. This relatively new method eliminates the need for a large abdominal incision. It also elimates the need to clamp the aorta during the procedure. Clamping the aorta creates significant stress on the heart and people with severe heart disease may not be able to tolerate this major surgery. Stent grafts are most commonly considered for patients at increased surgical risk due to age or other medical conditions.
Following aortic stent graft placement, patients are often discharged a day or two after interventional repair, and typically do not require an extensive ICU stay postoperatively. Once discharged, most return to normal activity within 2 weeks compared to 6 to 8 weeks after surgical repair.
If you have an abdominal aortic aneurysm and would like to obtain more information about non-surgical, minimally invasive repair, please contact MIIGS for a consultation with one of our physicians.
Overview
- AV Gortex Graft
- AV Fistula
- Tunneled Hemodialysis Catheter
- Temporary Hemodialysis Catheter
AV grafts and AV fistulas are used to provide access to hemodialysis in patients with end-stage renal disease. Grafts and fistulas serve as conduits from an artery to a vein. These conduits can become occluded or start functioning poorly during hemodialysis. When this happens, the graft or the native fistula can be re-opened or “tuned up” with minimally invasive techniques such as angioplasty or possibly stenting. Hemodialysis access can also be obtained by using a long-term tunneled hemodialysis catheter or a temporary catheter. MIIGS physicians can place both types of catheters, as well manage any complication such as; catheter malfunction, clotting, or slow flow.
Hemodialysis Access Management
The physicians at MIIGS have literally performed thousands of these procedures. Their expertise and proficiency in hemodialysis access management means you can resume dialysis in a timely manner, thereby decreasing any potential complications of end-state renal disease.
Overview
More than one-fourth of women and many men over the age of 65 will develop compression fractures in their vertebrae due to osteoporosis. These fractures are painful, and cause decreased mobility and accelerated bone loss. In addition, treatment can be very time consuming, uncomfortable and usually include long periods of bed rest, back braces and pain medication.
Vertebral Augmentation
Today, many seniors who suffer from these debilitating symptoms are candidates for two new treatments – Vertebroplasty and Kyphoplasty. Both of these minimally invasive procedures require only a small incision made at the site of the fracture. Vertebroplasty involves a process where bone cement is injected directly into the fractured bone. This stabilizes the fracture an in many cases provides immediate pain relief. Kyphoplasty involves an additional step. Prior to injecting the bone cement, a tiny balloon is inserted through a needle and gently inflated inside the fractured vertebrae. The balloon creates a pocket or cavity in the vertebrae. The balloon is removed and the bone cement is then injected into the space, filling the area.
Both of these procedures are painless, usually taking less than one hour to perform and relief can be expected almost immediately. Unlike traditional surgery, recovery time is much quicker, and 80-90% of patients report immediate relief from pain and 90-95% of our patients report complete relief from pain within 2 weeks.
MIIGS offers peripheral vascular disease (PVD) treatment in Alexandria, La., and surrounding areas. PVD treatment with MIIGS is minimally invasive and can prevent life-changing events, even at later stages. PVD, also known as peripheral arterial disease (PAD), is a very common condition affecting 12-20% of Americans age 65 or older. PVD develops most commonly as a result of atherosclerosis or “hardening of the arteries,” which occurs when cholesterol and scar tissue build up, forming a substance called plaque inside the arteries. This plaque narrows and clogs the arteries and is a very serious condition. The clogged arteries cause decreased blood flow to the legs, which can result in pain when walking and, if left untreated, can eventually lead to gangrene and possible amputation.
MIIGS physicians can open blood vessels at the site of blockages and restore normal blood flow using tiny catheters and other miniaturized tools and X-rays to perform these minimally invasive procedures.
If you think you may benefit from peripheral vascular disease treatment, discuss your symptoms with your physician, or simply contact one of our MIIGS physicians for a consultation by submitting a form or calling (318) 445-9700.
Overview
Peripherally Inserted Central Catheters (PICCs) are used to provide intermediate and long-term intravenous access for patients. The thinner veins in the arms may not be able to handle long-term intravenous treatment and PICCs are often used rather than traditional IVs.
Our skilled doctors placed this extremely thin catheter into the patient’s arm and then move it to the veins right above the heart, which are much larger and allow strong medications to be given without pain or damage to the smaller veins. Additionally, larger PICC lines can be used to draw blood samples without the need for additional needle sticks.
A Port is similar to other long-term IV lines, however, the entire device is buried underneath the skin. Ports are generally used in patients who require IV access for more than 3 months. A Port is placed directly into a central vein, usually in the neck or upper chest and the catheter proceeds to a position just above the heart. The catheter is then tunneled under the skin and the Port is secured against the chest wall through a separate incision (usually 1 to 2 inches in length).


